Pulmonary embolism, or PE, is a major cause of morbidity and death in the United States. In fact, about one in 1,000 people are affected by PE every year; some studies showing a nine-fold increase in the incidence of PE in patients with COVID-19. Unfortunately, the management of acute PE isn’t standardized across all of healthcare. And for all patients, unless otherwise contraindicated, prompt treatment with thrombolytic therapy is still the first-line recommendation.
However, with the advancement of technology and continued acquisition of new medical knowledge, classic approaches to PE treatment have changed. From the development of institutional PE teams, advancements in catheter-directed interventions, surgical therapies and the use of extracorporeal membrane oxygenation (ECMO) to improve patient outcomes, the PE landscape is blossoming.
Pulmonary Embolism Response Teams
Pulmonary embolism response teams (PERTs) first formed at Massachusetts General Hospital, with the goal of quickly and simultaneously engaging multiple clinicians from various specialty areas within the institution to determine the best course of action and care for patients with acute PE. Since its inception, many hospitals around the world have adopted this team approach intervention model. In fact, just a few short years after the first PERT was formed, the inaugural meeting of the National PERT Consortium was held. This consortium, which supports with setting guidelines and best practices for these institutionally based teams, describes that PERTS must meet the following criteria:
- Ability to rapidly assess and provide treatment for patients with acute pulmonary embolism
- A formal mechanism to exercise a full range of medical, surgical, and endovascular therapies
- Provide appropriate multidisciplinary follow‐up of patients
- If feasible, willingness to collect, evaluate, and share data regarding the effectiveness of treatment rendered
Most often, PERTs are called upon for patients who present with sub-massive or massive PE. However, these teams may also be consulted for low‐risk PE patients who have significant comorbidities, like an intracranial hemorrhage, and are not eligible to receive anticoagulant therapy.
Some study findings showed that the early utilization of PERTS resulted in improved patient outcomes, but additional research is needed to determine if this team approach improves survival rates, reduces long‐term complications of PE, and is cost‐effective to the institution and the patient.
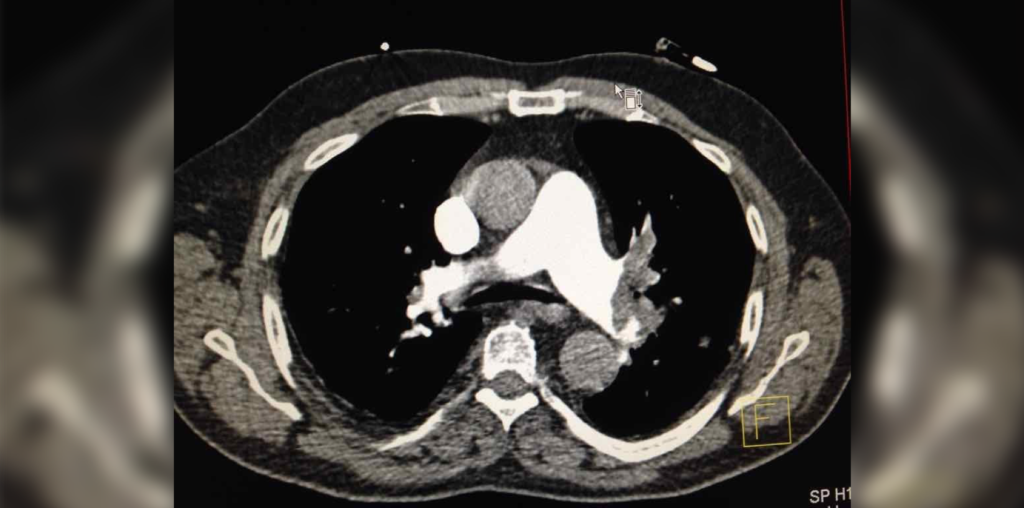
Catheter-Directed Interventions
Now, for intermediate- and high-risk PE patients, catheter-directed interventions are an alternative to classic systemic thrombolysis and is a minimally invasive alternative to surgical thrombectomy. Catheter-directed interventions include therapies that remove the blood clot alone, or in conjunction with catheter-directed thrombolysis (low-dose fibrinolytic agents directly injected into the pulmonary artery at a slow infusion rate, usually over 12–24 hours). This intervention is a good treatment option for a patient who cannot tolerate fibrinolysis but has a significant thrombosis. It’s important to note that with this intervention option, the location of the clot will determine the usefulness of catheter-directed interventions. For example, the PE must be proximal for the therapy to be effective.
Depending on the type of catheter-directed device used, the mechanism of action may be different:
- One catheter-directed intervention removes the thrombus by injecting a high-pressure jet of saline from the distal port, creating a negative pressure force. Simultaneously, another catheter helps remove the thrombus. However, as the thrombus breaks down, there could potentially be a sudden release of adenosine, which can cause hemodynamic decompensation.
- Another intervention uses a suction catheter alongside three mesh disks that help to completely evacuate any residual clot after the initial thrombus is removed using suction.
Catheter-directed therapies might also help normalize the pressure in the right side of the heart faster than anticoagulation. Though additional research is necessary, it’s an important finding as it may be the best intervention option for intermediate risk PE patients who are on the verge of rapid hemodynamic decompensation.
Surgical Therapies
Surgical pulmonary embolectomy can rapidly restore pulmonary blood flow and relieve acute obstruction. This surgical intervention historically has been the intervention of choice for:
- Patients with massive pulmonary embolism who cannot receive fibrinolysis or remain unstable after receiving fibrinolysis
- Patients with intermediate high-risk pulmonary embolism who either fail thrombolysis or have a contraindication
This surgical intervention is accomplished via a median sternotomy, and the patient must also be placed on cardiopulmonary bypass. Then, an incision is made through the pulmonary trunk and the main pulmonary arteries where the clot will be retrieved and removed.
Though this surgical approach has been associated with a higher mortality in the past, over recent years, it has been revised and standardized to reflect best practices to decrease the risk of perioperative mortality.
Hemodynamic Support
For patients with an acute PE and are hemodynamically compromised from a PE, venoarterial extracorporeal membrane oxygenation (VA-ECMO) may be recommended as an alternative means of circulatory support. Currently, guidelines recommend utilization of ECMO for “patients with acute high-risk pulmonary embolism and refractory shock with the caveat that it is used in combination with definitive therapy, such as surgical embolectomy or catheter-directed therapy”.
Studies around the early onset use of VA-ECMO show that it could be a potentially life-saving therapeutic option that can appropriately support the patient’s hemodynamics function long enough for the healthcare team to provide definitive therapy. Even with that said, it is still important to highlight that ECMO is associated with a high incidence of complications, such as bleeding and infection.
Published February 28, 2022
Join the Conversation
Register for Figure 1 and be part of a global community of healthcare professionals gaining medical knowledge, securely sharing real patient cases, and improving outcomes.