Summary
A 25-year-old man is in a rehab hospital following a hypoxic brain injury he sustained in a skiing accident. Several weeks into his recovery, he begins to experience clonic seizures of his left arm from one unusual trigger: Sudoku. Listen to the case that caught the attention of neurologists around the world.
Guests:

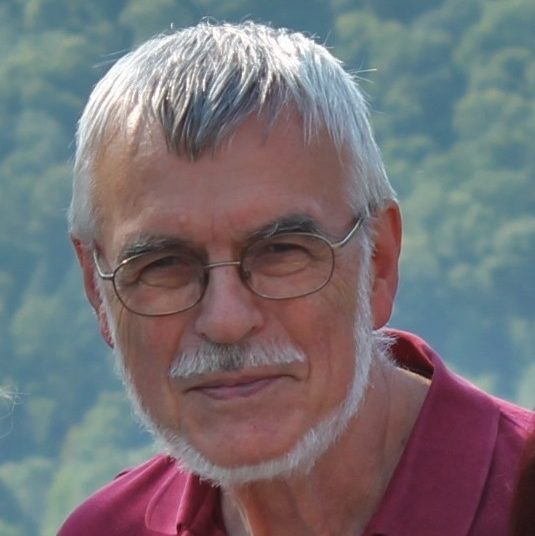
Berend Feddersen, M.D.
Dr. Feddersen is a neurologist and professor at the University of Munich in the department of neurology and department of palliative medicine. His research interests include status epilepticus, hypoxia at high altitude, and outpatient palliative care. In his spare time, he enjoys juggling.
Eter Wolf, M.D.
Dr. Wolf is a neurologist and leading epilepsy researcher. As initiator of the European Epilepsy Academy Eurepa, he developed widespread activities for professional education in epilepsy, including the establishment of the distance education system Virepa. His research interests include all clinical and comprehensive care aspects of epilepsy.
Resources:
- Ruptured mycotic aneurysm presenting as an intraparenchymal hemorrhage and nonadjacent acute subdural hematoma: case report and review of the literature
- Infectious Endocarditis Associated with Subarachnoid Hemorrhage, Subdural Hematoma and Multiple Brain Abscesses
- Neurologic Complications in Infective Endocarditis
Transcript
DDx SEASON 1, EPISODE 6 TRANSCRIPT
Sudoku seizures
RAJ: A 25-year-old man is in a rehab hospital after suffering brain damage during a ski vacation. Several weeks into his recovery, he starts to experience clonic seizures of his left arm.
Theme music
RAJ: This is DDx, a podcast from Figure 1 about how doctors think.
I’m Dr. Raj Bhardwaj.
Today’s case comes from Dr. Berend Feddersen.
FEDDERSEN: I’m a neurologist from Munich, Germany.
RAJ: This case involves a young man who was referred to Dr. Feddersen from an inpatient rehabilitation centre. Several weeks earlier, the man had almost died in an
avalanche.
FEDDERSEN: He was buried by an avalanche when he was skiing in the Alps. He was rescued after 15 minutes under the snow. He was resuscitated and he came with a helicopter to an emergency department.
After the first diagnostic tests and therapies, he went in a rehabilitation center. He had quite a lot of luck because he lived, and he had some small hypoxic brain injuries which led to these myoclonic jerks during activation of the mouth and the legs. He was treated with anti-epileptic medication.
RAJ: But it wasn’t the myoclonic seizures that led to Dr. Feddersen getting involved in this case.
The patient was recovering well, spending lots of time resting and doing physical therapy, when he started to notice a new kind of seizure.
FEDDERSEN: In the rehabilitation center, he had a lot of physio therapies and he was a little bit bored. So he was doing Sudoku puzzles in his free time. There were some clonic jerks of his left arm, which he couldn’t control.
RAJ: The strange thing about these new clonic seizures was that they only seemed to happen when the patient did sudoku puzzles. Not when he was doing crosswords. Not when he did math problems in his head. Just sudoku.
FEDDERSEN: I was very curious about these jerks and about the question, where they came from.
RAJ: Dr. Feddersen and his team decided to have the man do sudoku while he was hooked up to an EEG machine. As soon as the patient started doing the puzzles, his left hand and left arm started to twitch.
FEDDERSEN: And on the EEG we saw an epileptic seizure pattern on the right central parietal region.
RAJ: That part of the brain—the right central parietal lobe—is involved in processing visual and spatial information.
At first, Dr. Feddersen couldn’t figure out why solving sudoku, which are basically little math problems, would activate this part of the brain.
He asked the patient to explain exactly what was going on in his mind while he was doing the puzzles.
It turns out, the patient pictured sudoku numbers in a three-dimensional grid.
FEDDERSEN: He told me it was some kind of, um, imagination that this is in these rows, and in vertical columns. He imagined this sudoku puzzle as a three-dimensional figure to solve the problem.
RAJ: Dr. Feddersen was surprised to hear the patient’s explanation of how he did the puzzles.
It had never occurred to him to approach sudoku like that.
FEDDERSEN: I found it very interesting that there are people around in this world who are solving sudoku puzzles with the three-dimensional imagination. I tried this, but I was not successful.
I mean, when I have a sudoku puzzle, I just do the sudoku puzzle, I do it very differently I think than he did it because I just do the math in my mind.
RAJ: This detail about how the man solved the puzzles, proved to be an important clue about what was going on.
FEDDERSEN: Our brain uses a lot of the right central parietal region when we imagine things three-dimensionally.
We were testing for crosswords and for normal arithmetic tasks, but there he didn’t have any problems. It was really when he imagined things three dimensionally.
RAJ: So the connection to this part of the brain was starting to make a lot more sense.
They did a diffusion tensor imaging scan which revealed a complete loss of inhibitory fibres in the right central parietal lobe.
FEDDERSEN: Now we were sure what really happened when he was buried by the avalanche and he had these 15 minutes of hypoxia. He had a loss of inhibitory fibers, and when he was doing some kind of activation in this area, this led to an over activation resulting in an epileptic seizure with clonic jerks of the left arm.
We learned, from these results that if you have a loss of inhibitory activity in the brain and you have exactly in this region an activation—in this case with the three dimensional imagination—this can lead to very localized epileptic seizures.
RAJ: Dr. Feddersen suggested that from now on, the man could just try doing sudoku puzzles without thinking about them in 3D.
FEDDERSEN: He imagined this all the time in this three-dimensional manner, so that was a problem. So he was advised not to do any sudokus.
RAJ: And once he gave them up, the seizures disappeared.
RAJ: It ended up being a real-life example of the old joke, “Doc, it hurts when I do this!” “Well then, don’t do that.”
RAJ: When this case was published in JAMA Neurology in 2015, it caught the attention of neurologists all over the world.
Dr. Peter Wolf is a neurologist and epilepsy specialist in Denmark.
WOLF: In all my career I have been very much interested in what we call reflex epilepsies. That seizures are precipitated by some sensory input, or cognitive input.
RAJ: For Dr. Wolf, this case was a perfect example of how hard it can be to pin down the specific sensory triggers of these types of seizures.
WOLF: You could ask many neurologists, they would say reflexive epileptic mechanisms are relatively rare, but if you ask me, they are not, they are very frequent. You just have to be alerted to them; you have to be aware of them, and then you will see them everywhere.
RAJ: Dr. Feddersen says this case taught him an important lesson about listening to his patient, and trying to understand things from their point of view.
FEDDERSEN: I think it’s very important to listen closely to what patients are feeling. And I mean, in this case it was obvious that the left arm was shaking and he had these jerks, but sometimes we have reported problems from patients which we, sometimes in the first moment, we’re not sure if it’s real or not, but we should listen carefully to what the patients are saying.
RAJ: Dr. Wolf agrees that doctors should pay close attention to their patients’ impressions of what’s causing their seizures.
WOLF: I think the particular diagnostic challenge here is that many doctors would consider the report of a patient, that his seizures are precipitated by some particular input, would look at this as unimportant, circumstantial, perhaps not truly reliable. But, when you know about reflex epilepsies and about the generation of epileptic seizures in the brain, you would be alerted to this. And you would listen to what the patient tells you, because the patients knows so much. And if you don’t ask them, you will miss it.
Thanks to Dr. Berend Feddersen and Dr. Peter Wolf.
This is DDX, a podcast by Figure 1, the knowledge sharing app for doctors.
Figure 1 is an app that lets doctors share clinical images and knowledge about difficult-to-diagnose cases.
DDx is produced by Earshot Podcasts.
Sound design and mixing by Chandra Bulucon.
Our theme music is by Nathan Burley.
The executive producers of DDx are Jesse Brown and Corey Marr.
You can find links to Dr. Feddersen’s work and video of this patient’s sudoku-induced seizures at figure1.com/ddx. You can also see pictures of a surgery that stopped a musician’s seizures while preserving his ability to perform.
I’m Dr. Raj Bhardwaj. You can follow me on Twitter at @RajBhardwajMD.
Thanks for listening.