Treating wounds is complicated. These five medical cases shared by the Figure 1 community show how collaboration and resourcefulness are key to successful wound care.
#5.
A registered nurse shared these case details of a patient with quadriplegia presenting with an undiagnosed wound: “45yo quadriplegic male has developed wounds around urostomy … Wounds started approx. 6 years ago while hospitalized for flap surgery for pressure injury. New product was used around ostomy and wounds developed. Wounds increase and decrease in size but never close … Multiple wound treatments tried including silver, honey, steroids, collagen. Recent biopsy showed spongiosis and chronic inflammatory infiltrate with lymphocytes and eosinophils. Negative for bacteria, fungus, cancer and pyoderma gangrenosum.”
Unable to successfully identify or treat the wound, the registered nurse turned to the Figure 1 community for help. Treatment suggestions included applying a skin barrier protective sheet, a hydrocolloid skin plate, or collagen dressings.
What’s your diagnosis and treatment plan?
#4.

A patient presented with a two-month history of a leg wound with pus discharge to the family medicine physician who shared this case. During the visit, the patient remembered possibly having been stung or bitten while in Yemen around the time the lesion appeared.
A dermatologist who commented on the case offered the following, “Looks like multiple fistulae from a subcutaneous infection. Look for bacteria (pyogenic Gram+ and Gram-), mycobacteria (M. Ulcerans, Buruli Ulcer), fungus (mycetoma) and parasites (leishmaniasis). Sample the pus for culture, do biopsies to search for granulomas + PAS + Grocott + Zielhl. X ray or scan of the subcutaneous layers and bone.”
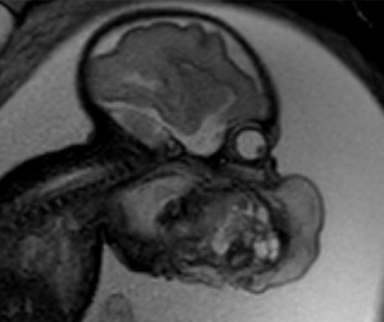
#3.

This third most interesting medical case shows the follow-up of a diabetic foot wound after being treated with non-medical grade honey. The community jumped in to share their surprise at the progress.
“It is looking AMAZING! I am so impressed … Keep up the great work!”
“I’m just speechless.”
See the wound prior to treatment
#2.

A registered nurse shared this medical case of an open wound following a fasciotomy to relieve compartment syndrome. The patient had been found down after as many as 12 hours. The registered nurse provided this update: “This patient would later require wound vac therapy, SLED dialysis for rhabdomyolysis and tracheostomy.” Fortunately, the patient’s wound was successfully closed.
What are your thoughts on the management of rhabdomyolysis?
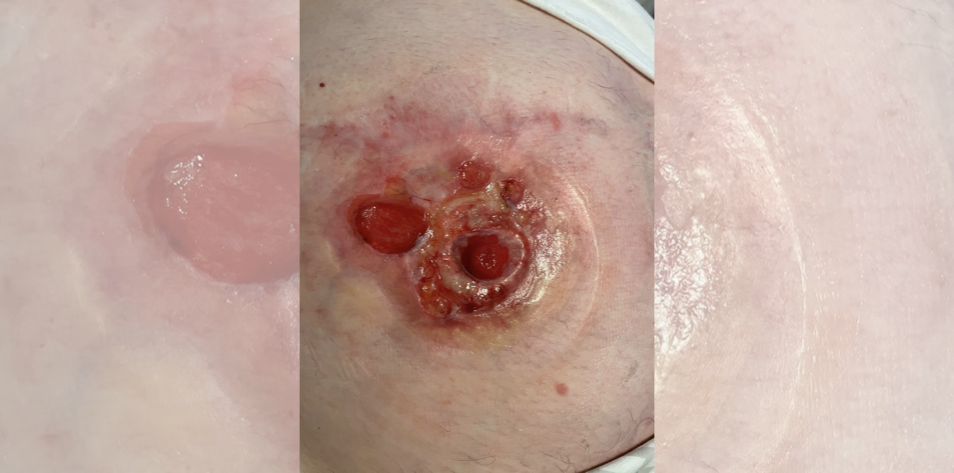
#1.

This medical case shows a necrotic wound on a patient’s breast following reconstructive surgery eight weeks prior. A plastic surgeon commented on the post, “She needs to see a plastic surgeon. It is imperative to know if there is an implant under there or is this autologous reconstruction. If no signs of spreading infection, would hold off on debridement until this information is known and the patient can see the appropriate specialist.”
The registered nurse who shared the case later provided this update: “[Incision and drainage] done to remove necrotic tissue. Given [antibiotics] and sent to a local plastic surgeon … She had implants underneath. The last I heard she was to get a new graft to form an areola after she heals.”
Published November 7, 2023
Join the Conversation
Sign up for Figure 1 and be part of a global community of healthcare professionals gaining medical knowledge, securely sharing real patient cases, and improving outcomes.