A 19-year-old patient presents to the emergency department with a recent history of increasing lethargy and polyuria. Over the past 24 hours, the patient’s condition has rapidly deteriorated including some episodes of vomiting, respiratory distress, and confused mental status. On examination, an elevated heart rate of 138 bpm is detected with a respiratory rate of 29 breaths per minute. Laboratory results reveal an alarming blood glucose level, elevated ketone levels, and a low serum bicarbonate level, reflecting a metabolic acidosis.
Diabetic Ketoacidosis
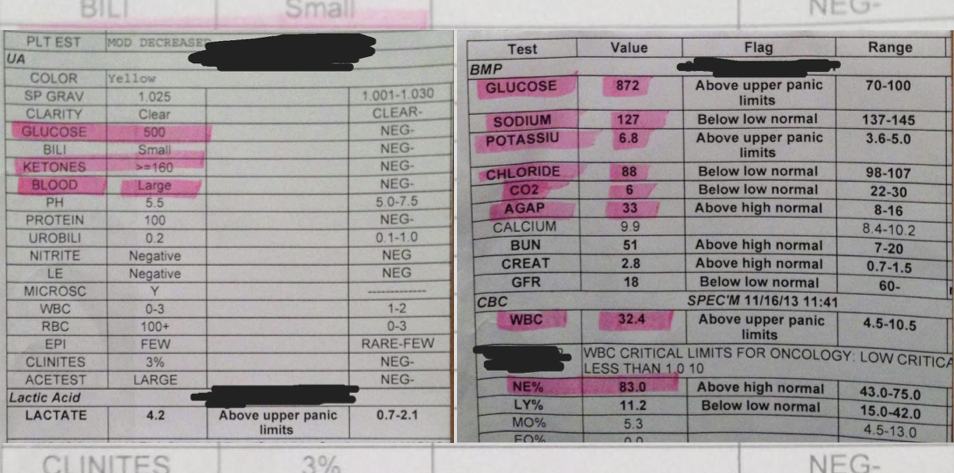
This patient is presenting a classic case of diabetic ketoacidosis, also referred to as DKA, a life-threatening complication normally found in uncontrolled diabetes mellitus, more frequently T1DM. DKA can develop in patients with diabetes due to a severe insulin deficiency, which leads to high glucose levels, and excessive ketone body production that is used as an energy source. The excessive level of ketone production can alter the acid-base balance, causing metabolic acidosis, marked by decreased pH levels in the blood pH, and low bicarbonate levels. Alternated osmolarity, decreased blood volume, and electrolyte imbalances are also significant findings that should be managed and monitored.
Symptoms
Individuals experiencing diabetic ketoacidosis commonly exhibit symptoms such as pronounced urination (polyuria), intense thirst (polydipsia), and variable alterations in mental status. The spectrum of mental status changes ranges from confusion to profound lethargy, and in severe critical cases, diabetic ketoacidosis can progress to a state of coma.
Management
The main goals of diabetic ketoacidosis management are correcting the hyperglycemia, decreasing the ketone body’s levels of ketosis, restoring the blood fluid, correcting the electrolyte imbalance, and preventing possible brain complications. The first intervention includes an aggressive intravenous fluid recovery with isotonic saline. Simultaneously, the use of insulin is started to promote glucose uptake from the cells, facilitating hyperglycemia control, and suppressing the formation of novel ketone bodies. In these cases, careful monitoring of signals, such as blood pressure, heart rate, respiratory rate, blood glucose levels, electrolytes, acid-base status, and urine testing is of key importance.
On the other hand, the treatment must be done with caution. Too aggressive insulin therapy can lead to hypoglycemia, also a potentially critical condition. Excessive use of intravenous fluid can lead to fluid overload, and the treatments aiming to address the electrolyte imbalance can lead to excessive intake.
It is important to highlight that severe diabetic ketoacidosis events can be prevented in patients with diabetes. However, the management of patients with diabetes depends on the collaborative efforts of a diverse team of professionals, including endocrinologists, nursing staff, nutritionists, and psychologists. Additionally, lifestyle modifications are also extremely relevant. Engagement in education about the condition and its treatment is a major point.
References
Figure 1 – The future of medical education [Internet]. [cited 2024 Jun 26]. Managing Heart Failure. Available from: https://app.figure1.com/cme/47ffe171-0eb4-47fc-9251-397f52c35333
Castellanos, Luz, et al. “Management of diabetic ketoacidosis in children and adolescents with type 1 diabetes mellitus.” Pediatric Drugs 22 (2020): 357-367.
Gosmanov, Aidar R., Elvira O. Gosmanova, and Erika Dillard-Cannon. “Management of adult diabetic ketoacidosis.” Diabetes, metabolic syndrome and obesity: targets and therapy (2014): 255-264.
Umpierrez, Guillermo E., and Abbas E. Kitabchi. “Diabetic ketoacidosis: risk factors and management strategies.” Treatments in endocrinology 2 (2003): 95-108.
Published July 10, 2024
Want more clinical cases?
Join Figure 1 for free and start securely collaborating with other verified healthcare professionals on more than 100,000 real-world medical cases just like this one.