A 56-year-old is brought to the emergency department after being found on the floor at work. The patient’s last known normal was two hours prior to arrival. They are alert but unable to follow most commands. They have complete expressive aphasia with limited comprehension. Cranial nerves are unremarkable except right nasolabial flattening. The patient can withdraw weakly in the right leg, but has no movement in the right arm. Their National Institutes of Health stroke score (NIHSS) is 16.
The patient’s local medical record shows no history of chronic conditions or medications. EKG shows atrial fibrillation. Blood pressure is 190/102 mmHg. A nicardipine drip is started with subsequent reduction in blood pressure into the 170s.
During an acute stroke, the body up-regulates blood pressure in an attempt to push collateral blood flow into the infarcted area. Therefore, blood pressure is lowered by the minimum necessary to decrease the risk of secondary hemorrhage into the stroke core.
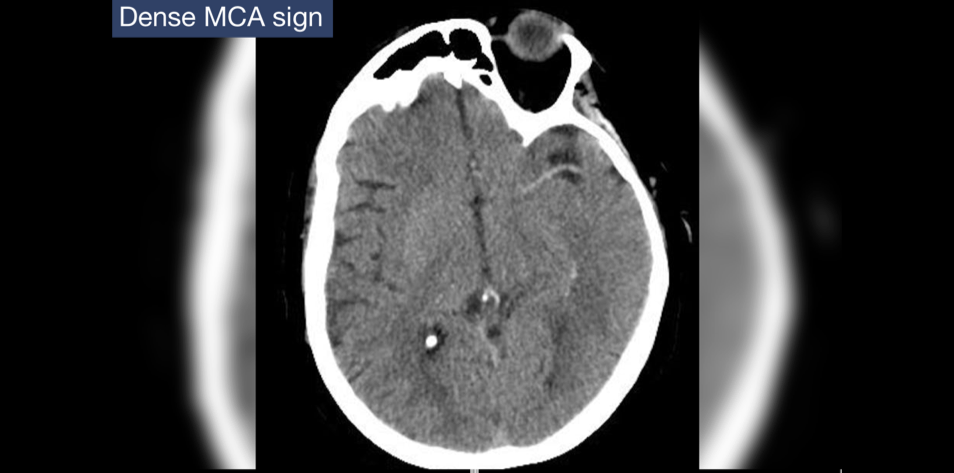
Platelets, glucose, and international normalized ratio (INR) are within normal limits. Head CT shows a dense MCA sign with no evidence of mass lesion or hemorrhage. An M1 occlusion is confirmed on CTA. CTP or emergent MRI is determined not to be necessary as the patient’s rapid presentation is well within the 4.5 hour maximum outlined by acute stroke management guidelines.
Emergency Mechanical Thrombectomy
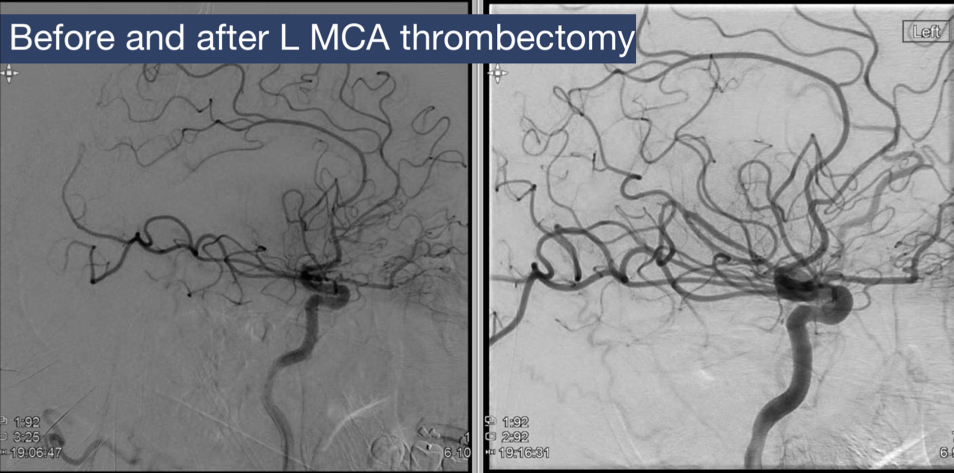
Although there is no way to confirm absence of recent surgery, use of anticoagulant that does not impact INR, or prior intracranial hemorrhage, the patient’s debility is significant enough that the team decides to proceed with IV thrombolytics, which are administered 2.5 hours after last known normal. The patient regains some arm movement in the right arm following initial bolus and is transferred emergently to a tertiary stroke center for mechanical thrombectomy. Near total revascularization is achieved.
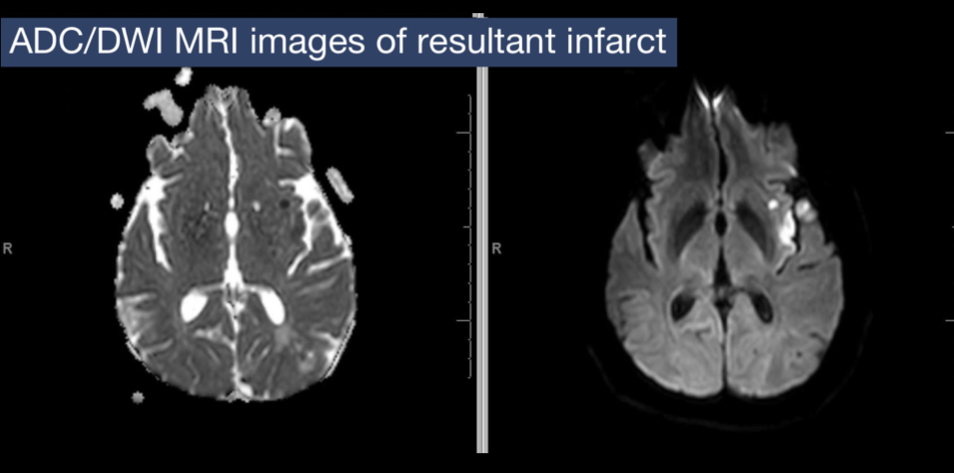
Immediately following the procedure, the patient regains anti-gravity strength on the right side, comprehension of simple verbal commands, and the ability to speak in simple phrases. Post-thrombectomy NIHSS score is 6. Follow-up CT is negative for signs of secondary hemorrhage. Follow-up MRI is pictured, revealing a relatively small area of infarction compared to the full MCA territory impacted prior to intervention.
Results of Etiologic Evaluation
A basic etiologic evaluation is completed including checking hemoglobin A1c, cholesterol, and an echocardiogram, which are unremarkable. Based on the size and location of the stroke, this is determined to be a cardioembolic stroke caused by the atrial fibrillation seen at the time of presentation.
Patient Outcomes
After one week, the patient is started on a direct oral anticoagulant for secondary stroke prophylaxis. Although there has historically been concern that starting anticoagulation too soon can cause post-stroke intraparenchymal hemorrhage, waiting longer than one to two weeks appears to increase the risk of recurrent stroke. High quality, randomized controlled trials are needed to confirm the optimal time to initiate, but current practice is about five days after infraction.
The patient is discharged to a facility for rehabilitation with good recovery potential. They are referred to follow up with cardiology and the outpatient stroke clinic.
References
Figure 1 – The future of medical education [Internet]. [cited 2024 Jun 26]. Management of Acute Ischemic Stroke. Available from: https://app.figure1.com/cme/40e57c63-55c0-463d-8141-219362deb33a
Kleindorfer DO, Towfighi A, Chaturvedi S, Cockroft KM, Gutierrez J, Lombardi-Hill D, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the american heart association/american stroke association. Stroke [Internet]. 2021 Jul [cited 2023 Jul 18];52(7). Available from: https://www.ahajournals.org/doi/10.1161/STR.0000000000000375
Seiffge DJ, Werring DJ, Paciaroni M, Dawson J, Warach S, Milling TJ, Engelter ST, Fischer U, Norrving B. Timing of anticoagulation after recent ischaemic stroke in patients with atrial fibrillation. Lancet Neurol. 2019 Jan;18(1):117-126. doi: 10.1016/S1474-4422(18)30356-9. Epub 2018 Nov 8. PMID: 30415934; PMCID: PMC6524642.

Kaci McCleary, MD
Hospice and Palliative Care Fellow, OhioHealth
Published July 24, 2024
Want more clinical cases?
Join Figure 1 for free and start securely collaborating with other verified healthcare professionals on more than 100,000 real-world medical cases just like this one.