Summary
A 45-year-old woman presents to the emergency department after experiencing an episode of acute abdominal pain and brief blindness in her right eye. Her symptoms have since resolved and she feels fine. She’s sure she is wasting emergency medicine physician Dr. Ashoo’s time. She isn’t.
Guests:

Sam Ashoo, M.D.
Sam Ashoo is a practicing emergency physician in the US (Florida). He is certified by the American Board of Emergency Medicine and is the author of www.admin-em.com. He has over 15 years experience in clinical practice and serves as a clinical assistant professor of emergency medicine at the Florida State University College of Medicine. In addition to teaching, he has a passion for medical administration and patient flow.

Marjorie P. Stiegler, M.D.
Dr. Stiegler is a Harvard-trained physician specializing in anesthesiology. Since 2005, her academic focus for research, writing, and speaking has been the application of behavioral psychology to patient safety in medical settings. She has given over 100 presentations across the globe on the role of cognitive bias in medical decision making, expertise, and error. Her publications can be found here. Dr. Stiegler also has a professional blog and can be followed on Facebook and Twitter at @drmstiegler. Her book “Quality and Safety in Anesthesia and Perioperative Care“ is available on Amazon.
Resources:
- Clinical, Diagnostic, and Management Perspectives of Aortic Dissection
- Acute Aortic Dissection: Clinician Update
- Guidelines for the Diagnosis and Management of Patients With Thoracic Aortic Disease
- Aortic Dissection: A 250-Year Perspective
- Decision-Making and Cognitive Strategies
Transcript
DDx SEASON 1, EPISODE 4 TRANSCRIPT
The near-miss
RAJ: A 45-year-old woman presents to the emergency department with no symptoms whatsoever. Her sudden-onset abdominal pain resolved an hour earlier. She apologizes for wasting everyone’s time because she’s pretty sure she’s fine. She isn’t.
Theme music
RAJ: This is DDx , a podcast from Figure 1, about how doctors think.
I’m Dr. Raj Bhardwaj.
Today’s case comes from Dr. Sam Ashoo.
ASHOO: I’m a board certified emergency physician in Florida, where I have been working for the past thirteen years.
RAJ: It was a routine evening in the emergency department when Dr. Ashoo picked up a patient who looked well – like maybe she didn’t need to be in the ED at all.
A quick note, the patient in this case is represented by a professional standardized patient, like the ones used in clinical training and exams.
ASHOO: When I went to question her about her symptoms, she said that she was at a local restaurant nearby and she started experiencing some abdominal discomfort.
SP up: I was sitting at the table, and then out of nowhere, I felt this sharp pain
It started in my stomach. But then it kind of shot up through my chest and into my neck. And then, all of a sudden, I couldn’t see anything out of my right eye. I was completely blind on one side.
It only lasted for a moment and then my sight came back, and I felt the pain go back down through my chest and into my stomach again, and then it disappeared.
I’ve felt completely fine ever since.
ASHOO: She had no symptoms. She said she felt rather silly for being there and making a big deal out of it, but she was with her husband who was concerned about her symptoms.
RAJ: While Dr. Ashoo was speaking with the patient, a nurse happened to be in the room doing vitals.
ASHOO: So the pulse rate was normal, but the initial blood pressure was not. It was at 88, over 42. So I asked the nurse to check the blood pressure in the other arm while I asked the patient about some other past medical history. She was otherwise healthy. She had no medications. She had no medical problems and had never had any surgeries, and really had never experienced anything like this before and she thought of herself as a pretty healthy person.
Meanwhile, the second blood pressure in the other arm was normal.
ASHOO: At that point I stopped to consider, but I really could only think of one that could cause all of her symptoms together.
RAJ: The discrepant blood pressure readings made aortic dissection shoot up to the top of Dr. Ashoo’s differential. Acute type A aortic dissection has a mortality rate of about 1% per hour initially.
Without treatment, the patient has a 50% mortality rate within 48 hours, and about 75% within the second week.
ASHOO: I tried to explain this to the patient, that I was the most concerned about aortic dissection. Uh, she kind of looked at me quizzically and I explained to her that either she had this or all of this constellation of findings was exceedingly bizarre and we weren’t going to come up with an answer. And she thought I was a little over reactive.
SP: I mean, it was probably just indigestion or something.
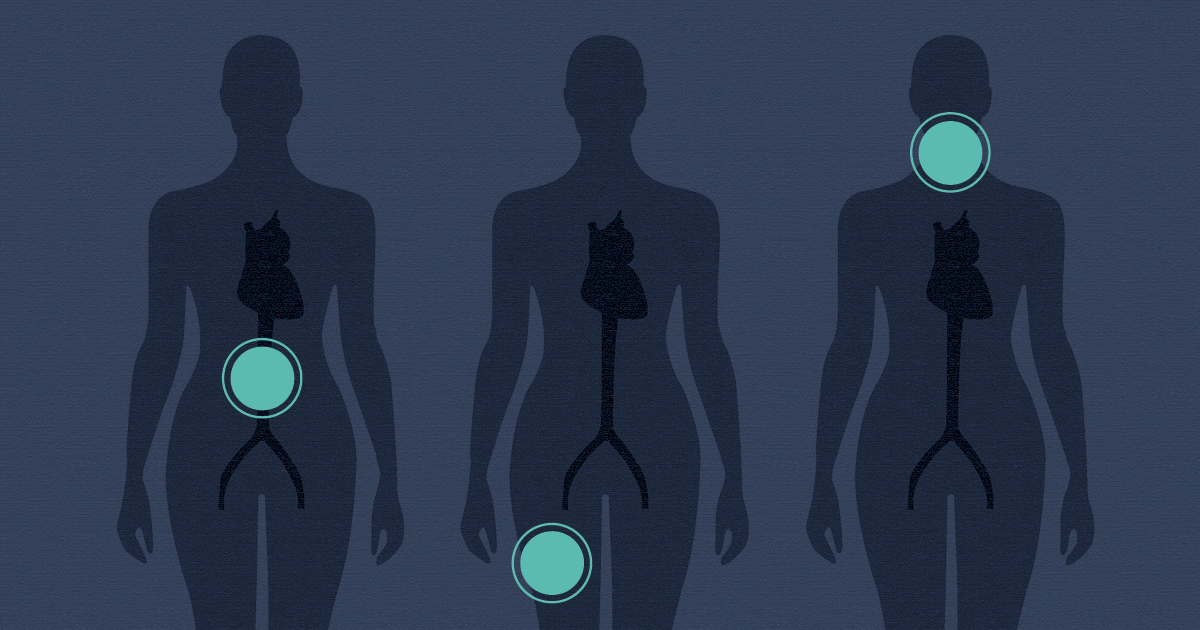
ASHOO: But we went ahead and performed a CT scan of her chest and abdomen with some IV contrast, and she had a type A, ascending dissection that began at the aortic root and traveled all the way down through her abdomen.
When I called our thoracic surgeon and explained the symptoms, she was rushed immediately to the operating room for a repair.
RAJ: The patient still felt fine and was asking to be sent home. Instead, she was heading into emergency surgery for a life-threatening condition. She was scared.
RAJ: The thoracic surgery team did an aortic valve replacement, and aortic endograft. The surgery was a success.
ASHOO: She did exceedingly well thankfully, and had no adverse reactions. And her postoperative course was unremarkable, and I’ve seen her since then and she’s doing very well and has no residual symptoms.
RAJ: Even though the patient made a full recovery, Dr. Ashoo was left rattled. If they hadn’t checked the blood pressure in both arms, they could have missed a serious diagnosis.
ASHOO: If she had told me she had previous vascular disease or surgery or she always had a low blood pressure or even if the blood pressures were symmetrical, I do often wonder, if the nurse had checked the right arm instead of the left arm first, and obtained a normal blood pressure, whether or not I would have actually pursued that diagnosis.
RAJ: That asymmetrical blood pressure pushed aortic dissection up to the top of Dr. Ashoo’s differential.
ASHOO: The classic description of how this presents in an emergency setting is the sensation of a tearing or sharp chest pain that radiates to the back that’s unrelenting and is very severe, and it’s typically described in patients who are exceedingly hypertensive, who may also complain of associated symptoms like shortness of breath or diaphoresis or nausea, but primarily this sharp intense, chest pain also felt in the mid-back.
RAJ: So this patient didn’t present with severe chest pain or any of the expected, most obvious symptoms of the disease. But that’s not the only reason Dr. Ashoo found this case a little odd.
You see, just a few months later, another woman came into the ED with unusual pain.
She was a previously healthy 65-year-old former ballet dancer, who passed out while running on her treadmill.
ASHOO: She arrived by ambulance to the emergency department once again without a complaint of chest pain, unusually complaining of severe leg pain. When I went to see her, she appeared very uncomfortable. Her countenance was not very good. She wasn’t very calm. Her skin color wasn’t normal and her blood pressure was low.
The one additional physical exam finding for her was she had very, very poor pulses in the right lower extremity. And once again she was emergently rushed to the CT scanner for an angiogram of the chest, and abdomen, and pelvis and in her case she also had a type A dissection beginning at the aortic root, traveling all the way down her aorta but also extending into her femoral artery on the right side, causing the ischemia of her right leg.
RAJ: OK, so that’s two aortic dissection cases in close succession. Both somewhat unusual presentations. Exact same diagnosis. Weird coincidence.
But then a few months later, a woman in her 40s shows up in the ER with chest pain and a history of migraines and hypertension.
ASHOO: At the time I was seeing her, her chest pain had improved but hadn’t actually completely resolved. It did not radiate to her back, but she did have throat pain, and the unusual characteristic here was instead of describing it as neck pain or upper back pain, she actually said I feel it in the front of my neck in my throat and I have a severe headache.
RAJ: Dr. Ashoo knew that aortic dissection was a possibility, but what were the chances? He thought maybe the symptoms could be related to her history of migraines, but there was this one other thing.
ASHOO: She did for a brief moment mention that she had some vision changes in her right eye.
She said well, it just seemed more bright in the right eye temporarily, and she once again was taken to the CT scanner for imaging of her chest, which did reveal the very same kind of type A ascending aortic dissection as we had in the other two cases.
This would be the third case now with some very atypical symptoms, all in women in the same age range with the exact same disease.
My conversations with my colleagues at that point were typically beginning with, ‘you’re never going to believe what I saw today.’ It was my third case in the last year and a half of this disease. It’s just very, very unusual.
RAJ: Getting a bunch of cases clustered together like this—the same, rare but life-threatening diagnosis—it’s hard not to let the diagnosis creep up your differential the next time you see a patient with similar symptoms.
ASHOO: So I think anytime that we see severe cases or a multitude of cases in a short period of time, we’re prone to bias. So what’s in my recent memory comes to mind pretty quickly, and absolutely, you know, as a human being, I’m certainly prone to that. Just like anyone else.
RAJ: The tendency for a diagnosis to come to mind more easily with future patients is called retrieval bias.
STIEGLER: So when Dr, Ashoo says he thinks that may affect how he practices in the future because of these three cases, that is likely to be true. It’s likely to be true now because they are recent cases, but it may be true even in the future because of the novelty of the cases. And he mentioned that psychological effect sort of of the near miss and the importance of getting these things right. And how, how they could have gone so wrong, and that is probably linked to a negative emotion for him, for just feeling the risk of possibly missing a diagnosis that has severe morbidity and mortality.
RAJ: This is Dr. Marjorie Stiegler, she’s an adjunct associate professor of anesthesiology at the University of North Carolina at Chapel Hill. She’s published extensively on cognitive biases in medicine.
STIEGLER: If you get any group of physicians together and you ask the question, have you been burned by something in your practice? This is sort of a phrase that I think resonates with everybody. Everyone has had an experience where they had a bad outcome and it changed their practice. So they say, you know, Oh, I’ve been burned before. So now I always check the blood pressure in both arms or I’ve been burned before, so now I never—fill in the blank, x, y, or z.
When physicians have these kinds of experiences, they absolutely do stick. And I’ve published several pieces about this, and gotten a lot of feedback from physicians.
RAJ: Since these three cases, Dr. Ashoo has caught himself looking a little harder for symptoms of aortic dissection, even though he knows that he’s no more likely to see a similar case now then he ever was.
ASHOO: I do tend to check bilateral arm blood pressures more often, I do tend to check pulses in extremities more often, and I do now tend to ask questions about neurological deficits. It is something I’m aware of but I don’t bring these three cases to scare everyone into ordering CT angiograms on every patient. It’s just finding the balance between how much in the way of diagnostic testing to order and what symptoms you can disregard is difficult, and that’s the art of medicine.
RAJ: Thanks to Dr. Sam Ashoo and Dr. Marjorie Stiegler.
This is DDx, a podcast by Figure 1, the knowledge-sharing app for doctors.
Figure 1 is an app that lets doctors share clinical images and knowledge about difficult-to-diagnose cases.
DDx is produced by Earshot Podcasts.
Sound design and mixing by Chandra Bulucon.
The executive producers are Jesse Brown and Corey Marr.
Our theme music is by Nathan Burley.
Dr. Sam Ashoo has shared more than 30 emergency medicine cases like this one on the
Figure 1 app. You can find links to those cases at Figure 1 dot com slash DDx and you can follow Dr. Ashoo on Figure 1 app at admin-EM.
I’m Dr. Raj Bhardwaj. You can follow me on Twitter at @RajBhardwajMD.
Thanks for listening.